Many of the researchers involved in the study take time out for a team photo. Photo Credit: Biernaskie lab
Researchers have used specialized genomic technology at the University of Calgary to enhance our understanding of Marjolin's ulcer (MU), a rare, highly aggressive skin cancer that may arise from established scars like those caused by severe burns.
"The longer you live with a chronic wound like a burn, the higher your risk of developing Marjolin's ulcer," says Dr. Jeff Biernaskie, PhD, principal investigator and Calgary Firefighters Burn Treatment Society Chair in Skin Regeneration and Wound Healing. "The more we know about underlying cellular interactions within the wound and how these cells are driven to become cancerous, the more likely we will be able to find a treatment which would be life-saving."

Lead author Sarthak Sinha.
The research team completed a cell-by-cell analysis to better understand how MU tumours grow. Using both single cell ribonucleic acid (RNA) sequencing and spatial transcriptomics available at UCalgary's Centre for Health Genomics and Informatics (CHGI), they did precise mapping of gene expression and cellular interactions within a tumor. With that enhanced view the researchers could trace how a small subtype of skin cells (keratinocytes) switch their function to start behaving like a type of support cell (fibroblast) that creates the conditions that encourage tumor cells to grow.
"The cancerous keratinocytes appear to undergo a career change,' shifting from their original role as outer skin cells to adopting new characteristics resembling dermal fibroblasts, which are the support cells found deeper in the skin," says Sarthak Sinha, MD/PhD candidate and lead author. "This transformation also enables them to start producing a type of extracellular matrix that is similar to what is found in developing skin. This new matrix essentially acts like fertile soil, creating the perfect environment for the cancer cells the seeds to take root, grow aggressively and spread to nearby structures.
"It's this interaction between the seed' and the soil' that may drive the tumour's invasive behavior. We believe this process plays a role not only in Marjolin's ulcer but also in other skin cancers, contributing to poor patient outcomes."
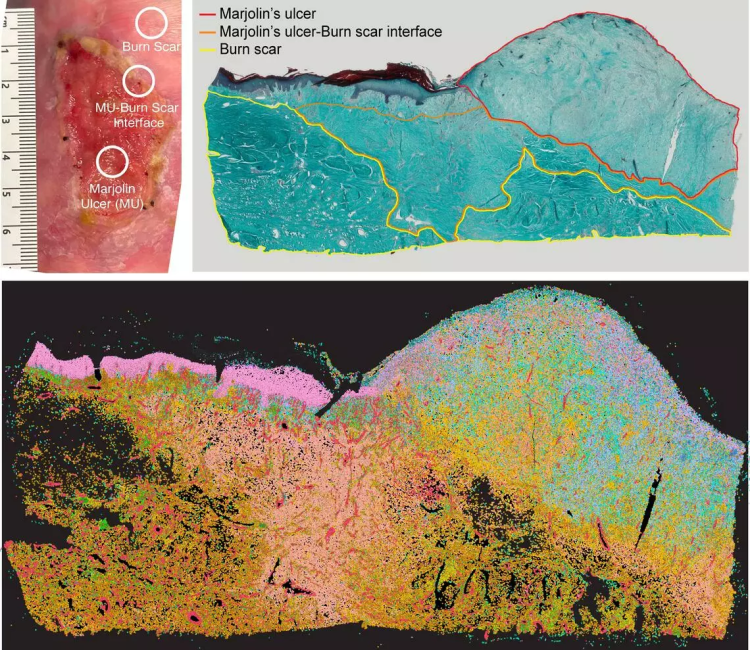
Image above, top left: Clinical photograph depicts Marjolin's ulcer (MU) emerging from burn scar. Top right: Histological section showing the transition from burn scar tissue to MU. Bottom: Spatial genomic imaging reveals the distribution of various cell types at the microscopic level. Each color corresponds to a different cell population, offering insights into the cellular milieu of MU and its progression from the adjacent scar tissue.
Dr. Vincent Gabriel, MD, medical director of the Calgary Firefighters Burn Treatment Centre, says insight into how these tumours start and thrive may also help to identify potential treatments to try to prevent the tumour from metastasizing.
"This study identifies opportunities for targeting the process that leads to Marjolin's cancer itself. A combination of surgical excision and medical intervention may limit the effect of these aggressive tumours," says Gabriel, who is also an associate professor at the Cumming School of Medicine and co-author of the study. "Successful treatments could offer greater peace of mind to burn survivors, especially those who may be highly prone to these cancers, providing significant relief after their challenging medical journeys."
Gabriel says MU can also be difficult to diagnose because a biopsy of the wound can miss the cancerous cells that are not uniform within the wound. The researchers say it is gratifying to share what they've learned with the hope someone will take it and learn more to help those diagnosed with aggressive skin cancers. The findings are published in the Journal of Investigative Dermatology.
The research was supported by the Department of Surgery's Surgical Research Development Fund and Calgary Firefighters Burn Treatment Society.
Co-authors of the study include Dr. Nicole Rosin, PhD; Rohit Arora, PhD candidate; Eren Kutluberk, PhD candidate; Dr. Myriam Verly, MD; Caleb Small, BHSc student; Aydin Herik, MD candidate; Lindsay Burnett, nurse practitioner; Leslie Cao, biomedical engineering student; Varsha Manoharan, PhD Candidate; Keerthana Chockalingam, BHSc student; Dr. Marieta van der Vyver, MD; Dragana Ponjevic, researcher; Dr. Holly Sparks, DVM, PhD; Dr. Sorana Morrissy, PhD; Dr. Ana Nikolic, MD, PhD; Dr. Robertson Harrop, MD; Dr. Thomas Brenn, MD, PhD; and Dr. Claire Temple-Oberle, MD.
Jeff Biernaskie is a professor in the Faculty of Veterinary Medicine and director of the Centre for Cell Therapy Translation. He is a member of the Alberta Children's Hospital Research Institute (ACHRI) and the Hotchkiss Brain Institute at the Cumming School of Medicine (CSM) and the Calgary Firefighters Burn Treatment Society Chair in Skin Regeneration.
Vincent Gabriel is an associate professor in the departments of Surgery and Clinical Neurosciences at CSM and member of the ACHRI and McCaig Institute for Bone and Joint Health at the CSM. He is a fellow of the American Burn Association and medical director of the Calgary Firefighters Burn Treatment Centre.
Sarthak Sinha is a post-doctoral scholar, MD-PhD Candidate in the Leaders in Medicine program class of 2025 at the Cumming School of Medicine, and a recipient of a Vanier, Alberta Innovates and Killam Scholarships.










